 An area of breastfeeding that gets little attention - but impacts an astoundingly large number of women - is the experience of sexual abuse survivors.
An area of breastfeeding that gets little attention - but impacts an astoundingly large number of women - is the experience of sexual abuse survivors.
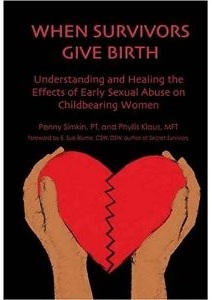
When I spoke with Penny Simkin, author of When Survivors Give Birth, for a podcast interview on breastfeeding and early sexual abuse, she estimated that between 25% and 40% of all women may be survivors of early sexual abuse.
So a new study by Dr. Kathleen Kendall-Tackett, which investigates the sleep disturbance and depression risk of sexual assault survivors in the first year after a child is born, has tremendous implications.
Research tells that women with a history of sexual assault are at higher risk for sleep difficulties and depression in general and also in the first year having a baby. But it also tells us that exclusive breastfeeding improves sleep and lowers risk of depression among women generally. And although some assume that sexual assault survivors would not want to breastfeed, they do breastfeed at rates comparable to non-survivors.
So the question Dr. Kendall-Tackett and her co-authors asked in this new paper was: does breastfeeding protect women with a history of sexual abuse from sleep disturbance and depression?
I’ll admit that when I first learned the subject of this study, I thought that the news would be bad. It reminded me of a story Penny Simkin told during our interview. She recalled a breastfeeding mother who had survived early sexual abuse. This mother found herself very disturbed by night feedings. Her abuse had taken place at night, and being awakened by her baby to feed at night was eliciting disturbing feelings related to the abuse. The solution they found? Set an alarm clock. Once the mother was awakened by the clock instead of a person, she was able to feed her baby at night without distress.
So, what did this new study find?
Dr. Kendall-Tackett and her co-authors examined the data collected through a large (over 6,000) survey of new mothers. Of the respondents, nearly 1,000 reported having experienced sexual assault (including early sexual abuse). Twenty five percent of the mothers reported childhood sexual abuse, but for this article the researchers only included those whose childhood experience included rape (about 3% of the sample) and those who reported sexual assault as teens or adults. These experiences have been shown to have more long term effects.
Consistent with prior research, survivors were as likely to breastfeed as non-survivors. And then they looked at three categories of infant feeding: breastfeeding (exclusive breastfeeding), mixed feeding, and formula feeding.
As expected, they found that women who had a history of sexual assault had a number of sleep difficulties (less hours of sleep, more time to fall asleep), increased risk of depression, and overall poorer well-being than non-survivor mothers.
“However,” the authors found, “sexual assault survivors who were [exclusively] breastfeeding were at lower risk on all of the sleep and depression parameters than sexual assault survivors who were mixed or formula feeding.”
These are associations, of course, and we can’t say with certainty that breastfeeding was the factor that “erased” the increased risk survivors face compared to non-survivor peers. Indeed, the authors state, “breastfeeding did not take away all of the negative effects of sexual assault.” But it did appear to substantially lessen them.
Prior research has drawn very clear connections between breastfeeding and lowered risk of depression and better sleep quality, so this is a reasonable connection to make. And there is a biologic model established by other research: “breastfeeding’s down-regulatory impact on the stress response.”
And as Penny Simkin pointed out in our interview, breastfeeding can be a healing act for some sexual abuse survivors, establishing a new connection with their bodies and empowering them as mothers. Perhaps this is evidence of more ways in which it heals.
For more information on Dr. Kendall-Tackett’s work on trauma and health, see her website. Her new book, Treating the Lifetime Health Effects of Childhood Victimization, 2nd Edition, (Civic Research Institute) will be available this year.











Twenty five percent of the mothers reported childhood sexual abuse, but for this article the researchers only included those whose childhood experience included rape (about 3% of the sample) and those who reported sexual assault as teens or adults. These experiences have been shown to have more long term effects.
*shakes her head* Sorry. Lost me there!
Yes, that part was confusing to me at first!
The authors only looked at survivors of abuse which involved (sorry to be graphic here) any kind of penetration, because the existing research showed that survivors of that kind of abuse were more likely to be exhibiting measurable symptoms (depression, sleep disturbance) as adults. And since the breastfeeding women in the survey were adults, it was important to be looking at a group who were likely to be showing symptoms to measure the effects of breastfeeding on those symptoms. They could have used the larger group of survivors, but then they were less likely to see symptoms, and then might not have been able to measure the effects of breastfeeding on those symptoms. Do you see why that makes sense as a design?
This is in no way to suggest that survivors of abuse which didn’t involve penetration don’t suffer long term effects of abuse. And it would be very interesting to see the level of adult symptoms among these women, and if they are widespread enough to measure whether breastfeeding might have an effect.
Thanks for the question - it was one that took me a bit to understand when I first read the study!
Sorry about that. I didn’t mean to lose anyone.
For these set of analyses, we opted to use the most serious form of child sexual abuse/sexual assault: contact that actually included oral, anal, or vaginal penetration. The reason for that is that this is the group that tends to have the most severe long-term symptoms. People who experience other types of contact child sexual abuse can also be quite symptomatic. But in the literature, abuse with penetration tends to be related to the most severe and long-lasting symptoms.
I hope that answers your question.